Brain Fog After Eating: 7 Foods Triggering Your Mental Fog
Experiencing mental cloudiness, difficulty concentrating, or energy crashes 30-90 minutes after meals? Discover the 7 foods causing postprandial brain fog and reactive hypoglycemia—plus a science-backed 2-week elimination protocol to restore mental clarity.
What is Postprandial Brain Fog?
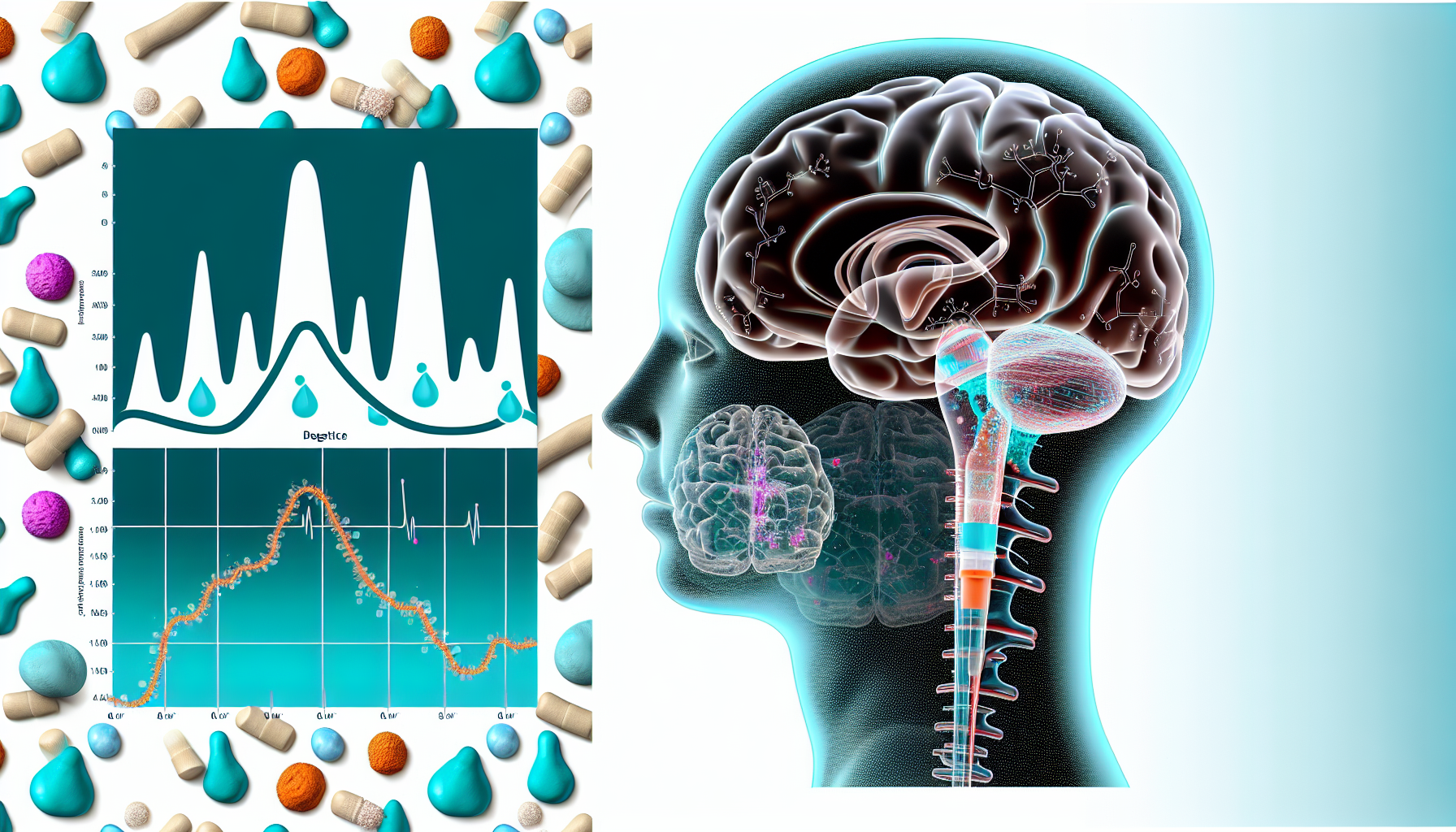
Postprandial brain fog refers to the onset of mental cloudiness, difficulty concentrating, slowed cognitive processing, and fatigue that occurs specifically after eating—typically within 30 minutes to 6 hours of a meal. Unlike general brain fog which may be constant, postprandial cognitive impairment is temporally linked to food intake and specific dietary triggers.
Why Does Food Cause Brain Fog?
The brain, despite being only 2% of body weight, consumes approximately 20% of the body's glucose and is exquisitely sensitive to metabolic disruptions. When you eat certain foods, several mechanisms can impair cognitive function: blood glucose crashes (reactive hypoglycemia), inflammatory cascade activation, blood-brain barrier disruption, neurotransmitter dysregulation, and histamine accumulation.
Key Characteristics of Postprandial Brain Fog:
- Temporal relationship to meals: Symptoms appear 30 min-6 hours after eating specific foods
- Mental fatigue and cloudiness: Feeling like thinking through fog or mental molasses
- Difficulty concentrating: Inability to focus on tasks that normally require minimal effort
- Energy crashes: Sudden onset fatigue despite having just eaten (paradoxical given food should provide energy)
- Slowed processing speed: Taking longer to understand information or respond to questions
- Word-finding difficulty: Inability to recall simple words or names during conversation
- Physical symptoms: Often accompanied by bloating, digestive discomfort, or drowsiness
Important distinction: Postprandial brain fog is different from normal post-meal drowsiness. Normal postprandial dip in alertness is mild and universal. Pathological postprandial brain fog is severe, impairing work performance, and indicates underlying metabolic or inflammatory dysfunction requiring intervention.
The 7 Foods Triggering Brain Fog (Scientific Mechanisms)
Based on peer-reviewed research from 2015-2025, these seven food categories are the primary culprits behind postprandial cognitive impairment. Each operates through distinct biological mechanisms affecting glucose regulation, inflammation, or neurotransmitter function.
Evidence: CGM studies show glucose nadirs averaging 65 mg/dL within 90 minutes after high-GI meals, correlating with cognitive impairment onset
Evidence: 89% of celiac patients and 95% of NCGS patients report gluten-induced neurocognitive impairment (GINI). Zonulin binds EGFR/PAR2 receptors, disrupting tight junctions
Evidence: 2025 review in Nutrition Reviews confirms A1 casein-derived peptides increase gut inflammation and modulate cognitive function. 64% of dairy-sensitive individuals report improved clarity after elimination
Evidence: Excitotoxins increase neuronal firing rate, leading to cellular exhaustion. Hidden in 'natural flavoring,' 'yeast extract,' 'hydrolyzed protein'
Evidence: Excess histamine activates H3 autoinhibitory receptors in brain, causing 'shutdown' and fog. Associated with ASD, fibromyalgia, MCAS, POTS
Evidence: 50% of AUD patients show detectable cognitive impairment. Causes 73% brain dehydration effects, white matter damage, and Wernicke-Korsakoff risk with chronic use
Evidence: 2022 meta-analysis shows low-GI meals favor cognitive function. High-GL diets associated with poorer MMSE scores in elderly. Late postprandial period (75-225 min) shows greatest cognitive impact
Science-Backed Mechanisms: How Food Causes Brain Fog
Understanding the biological pathways through which food affects cognition allows for targeted interventions. These four primary mechanisms explain the majority of postprandial brain fog cases.
Mechanism Explanation:
High-carbohydrate meals trigger excessive insulin release, causing blood glucose to plummet below 70 mg/dL within 90 minutes. The brain, consuming 20% of body's glucose despite being 2% of body weight, experiences immediate energy deficit.
Biomarkers:
Glucose <70 mg/dL, Insulin spike >30 μIU/mL
Research Evidence:
CGM studies show glucose nadirs at 30-90 min post-high-GI meals correlate with cognitive impairment. Occurs in idiopathic (180 min), alimentary (120 min), and late (240-300 min) forms
Clinical Severity: Acute cognitive dysfunction is immediate; recovery can be delayed despite glucose normalization
Mechanism Explanation:
Gluten triggers zonulin release in genetically susceptible individuals. Zonulin binds EGFR and PAR2 receptors on tight junction proteins, causing cytoskeletal rearrangement and junction disassembly in both gut and blood-brain barrier.
Biomarkers:
Serum zonulin >100 ng/mL, Anti-gliadin IgG
Research Evidence:
Brain endothelial cells express zonulin receptors. Elevated zonulin facilitates neuroinflammatory molecule penetration. Zonulin levels correlate with cognitive deterioration in CNS diseases
Clinical Severity: 89% CD patients, 95% NCGS patients report GINI (difficulty concentrating, forgetfulness, grogginess)
Mechanism Explanation:
Food sensitivities trigger IgE, IgG1, IgG2a antibodies, activating mast cells which release histamine, proteases, leukotrienes, prostaglandins, and TNF-α. These cross compromised BBB, activating microglia and causing neuroinflammation.
Biomarkers:
TNF-α elevation, IL-6, IL-1β, chymase
Research Evidence:
Food allergy increases TNF-α in serum and brain (cerebral cortex, hippocampus). Impairs motor activity and object recognition memory. Chronic inflammation creates escalating neuroinflammation cycle
Clinical Severity: Leukocyte CNS infiltration increases significantly during food reactions
Mechanism Explanation:
Multiple mechanisms disrupt neurotransmitter balance: alcohol enhances GABA while blocking glutamate; casomorphins bind opioid/dopamine receptors; histamine dysregulates dopamine and serotonin; excitotoxins overstimulate glutamate receptors causing neuronal exhaustion.
Biomarkers:
Altered dopamine, serotonin, GABA, glutamate ratios
Research Evidence:
Casomorphins demonstrate opioid-like effects. Excess histamine activates H3 autoinhibitory receptors. MSG causes neuron exhaustion via overstimulation
Clinical Severity: Immediate impact on cognition, mood, focus, and mental clarity
The 2-Week Elimination Protocol (Evidence-Based)
Systematic 2-week protocol to identify trigger foods causing postprandial brain fog. Based on clinical elimination diet guidelines (NIH, Cleveland Clinic, StatPearls 2024).
Foods to ELIMINATE:
- ✗All gluten (wheat, barley, rye, oats unless certified GF)
- ✗All dairy (milk, cheese, yogurt, butter, whey, casein)
- ✗All added sugars and refined carbs (white bread, pasta, pastries, candy)
- ✗Processed foods with additives (MSG, artificial sweeteners, preservatives)
- ✗High-histamine foods (aged cheese, fermented foods, alcohol, cured meats)
- ✗Alcohol (all forms)
- ✗High-GI foods (white rice, potatoes, corn flakes, instant oats)
Foods ALLOWED:
- Clean proteins: wild fish, grass-fed meat, pasture-raised poultry, eggs (if tolerated)
- Non-starchy vegetables: leafy greens, cruciferous, zucchini, peppers, cucumber
- Low-GI carbs: quinoa, sweet potato, lentils, chickpeas, steel-cut oats (GF)
- Healthy fats: avocado, olive oil, coconut oil, nuts (except peanuts), seeds
- Fresh fruits (low-GI): berries, green apples, pears, citrus
- Herbs and spices: turmeric, ginger, garlic, basil, oregano
Protocol Rules:
- 1.Eat every 3-4 hours to maintain glucose stability
- 2.Each meal must include protein (20-30g) + healthy fat + fiber
- 3.Drink 2-2.5L water daily (front-load morning/afternoon)
- 4.Track symptoms in food diary: time, food, symptoms, severity (1-10), onset time
- 5.Monitor energy, focus, mood, digestive symptoms
Expected Outcomes:
Days 3-5: Possible withdrawal symptoms (headache, irritability, cravings). Days 5-7: Symptoms begin clearing, mental clarity improves, energy stabilizes
Reintroduction Schedule:
Reintroduce: Gluten
Protocol: Day 8 morning: 1 slice whole wheat bread. Day 8 lunch: pasta. Monitor for 72 hours. Note symptoms at 2hr, 6hr, 24hr, 48hr, 72hr
Watch for: Brain fog, headache, digestive issues, joint pain, fatigue
Reintroduce: Dairy (if gluten was tolerated)
Protocol: Day 11 morning: 8oz milk or yogurt. Day 11 afternoon: cheese. Monitor for 72 hours
Watch for: Mental sluggishness, congestion, digestive distress, skin reactions
Reintroduce: High-GI carbs (if previous foods tolerated)
Protocol: Day 14 morning: white bread or white rice. Monitor glucose response and cognitive symptoms
Watch for: Energy crash, difficulty concentrating 30-90 min post-meal
Protocol Rules:
- 1.Only reintroduce if feeling well - if symptoms persist, extend elimination
- 2.Reintroduce ONE category at a time with 3-day spacing
- 3.Eat significant portion (2-3 servings) to trigger response
- 4.If symptoms appear, stop that food and wait until clear before next reintroduction
- 5.Continue detailed food diary documentation
How to Interpret Results:
Symptoms within 2-6 hours = likely trigger. Symptoms at 24-72 hours = delayed sensitivity. No symptoms after 72 hours = likely tolerated
Success with the elimination protocol requires meticulous tracking. Download our comprehensive food diary template (PDF + Excel) that includes: daily meal logs with timestamps, symptom severity tracking (1-10 scale), glucose readings section (if using CGM), sleep and stress logs, reintroduction challenge worksheets, and weekly pattern analysis summaries.
Glucose-Stabilizing Meal Combinations
These 10 meal and snack combinations are specifically designed to prevent reactive hypoglycemia, maintain stable blood glucose for 3-5 hours, and provide sustained cognitive energy. Each includes balanced macros, glycemic index data, and timing recommendations based on chronobiology research.
Foods:
3 eggs scrambled in olive oil + 1 cup sautéed spinach + 1/2 avocado + 1/2 cup berries
Protein: 25g | Fat: 28g | Carbs: 15g (fiber: 9g) | GI: <40
Glucose Impact:
Peak glucose: +20-30 mg/dL at 60 min, stable for 3-4 hours. No reactive hypoglycemia
Timing: Eat within 1 hour of waking to stabilize cortisol-glucose axis
Foods:
Greek yogurt (if dairy tolerated) or coconut yogurt + 1/4 cup walnuts + 1 Tbsp chia seeds + 1/2 cup blueberries + cinnamon
Protein: 20g | Fat: 18g | Carbs: 22g (fiber: 8g) | GI: <45
Glucose Impact:
Cinnamon improves insulin sensitivity. Protein + fat blunt glucose spike. Gradual rise over 90 min
Timing: Ideal for those who prefer lighter breakfast. Pair with 10-15g additional protein if very active
Foods:
Wild salmon (6oz) + quinoa (3/4 cup cooked) + roasted vegetables (broccoli, bell peppers) + olive oil + turmeric dressing
Protein: 42g | Fat: 18g | Carbs: 35g (fiber: 7g) | GI: <55
Glucose Impact:
Omega-3 fatty acids reduce neuroinflammation via HMGB1/TLR4/NF-κB pathway. Stable glucose 4-5 hours
Timing: Lunch at consistent time daily (±30 min) enhances metabolic regularity
Foods:
Grass-fed beef or turkey burger (no bun) + sweet potato (1/2 medium) + large salad with olive oil + apple cider vinegar dressing
Protein: 35g | Fat: 16g | Carbs: 28g (fiber: 6g) | GI: <60
Glucose Impact:
Apple cider vinegar reduces postprandial glucose by 20% when consumed with meals. Sweet potato provides sustained energy
Timing: Ideal 4-5 hours after breakfast to maintain glucose stability throughout afternoon
Foods:
Pasture-raised chicken (6oz) + lentils (1 cup cooked) + sautéed kale with garlic + 1/4 avocado
Protein: 48g | Fat: 14g | Carbs: 32g (fiber: 12g) | GI: <50
Glucose Impact:
High fiber load (12g) slows glucose absorption. Protein prevents overnight hypoglycemia. Stable through sleep
Timing: Eat 3-4 hours before bed to optimize sleep while maintaining glucose stability
Foods:
Apple slices + 2 Tbsp almond butter + sprinkle of cinnamon
Protein: 8g | Fat: 16g | Carbs: 18g (fiber: 5g) | GI: <40
Glucose Impact:
Fat + protein prevent glucose spike from apple. Sustains energy 2-3 hours
Timing: Use between meals if gap exceeds 4-5 hours or if experiencing early hunger/fog signals
Foods:
1/4 cup mixed nuts + 1/4 cup blueberries + 1 oz dark chocolate (85%+)
Protein: 7g | Fat: 20g | Carbs: 15g (fiber: 5g) | GI: <45
Glucose Impact:
Dark chocolate flavanols improve cerebral blood flow. Minimal glucose impact with sustained energy
Timing: Afternoon option when mental fatigue appears but dinner is 2+ hours away
Foods:
2 hard-boiled eggs + 1/2 cup raw veggies (carrots, cucumber) + 10 olives
Protein: 14g | Fat: 14g | Carbs: 8g (fiber: 3g) | GI: <30
Glucose Impact:
Provides sustained energy without glucose volatility during exercise. Consumed 60-90 min pre-workout
Timing: Morning or afternoon workout fuel. Low-carb prevents exercise-induced hypoglycemia in sensitive individuals
Foods:
Turkey roll-ups: 4oz sliced turkey + cucumber + avocado + mustard in lettuce wraps
Protein: 32g | Fat: 12g | Carbs: 6g (fiber: 4g) | GI: <25
Glucose Impact:
Minimal carb load prevents bedtime glucose spike. Protein prevents nocturnal hypoglycemia
Timing: Light dinner option or late evening snack if dinner was early. Supports overnight glucose stability
Foods:
Protein powder (20g) + 1 cup spinach + 1/2 cup berries + 1 Tbsp flax + 1/2 avocado + unsweetened almond milk + turmeric + ginger
Protein: 25g | Fat: 16g | Carbs: 18g (fiber: 10g) | GI: <40
Glucose Impact:
Turmeric + ginger reduce inflammation. High fiber slows absorption. 3-4 hour glucose stability
Timing: Quick breakfast alternative or post-workout recovery within 30-60 minutes
- Protein minimum: 20-30g per meal to prevent glucose crashes and maintain neurotransmitter synthesis
- Healthy fats: 10-20g per meal to slow gastric emptying and blunt glucose spikes
- Fiber target: 5-10g per meal to modulate glucose absorption and support gut microbiome
- GI limit: Keep total meal glycemic index below 55 for optimal glucose stability
- Meal frequency: Eat every 3-4 hours (never exceed 5 hours between meals during waking hours)
Tools & Technology to Identify Your Triggers
While the elimination protocol is the gold standard for identifying food sensitivities, these evidence-based tools can accelerate diagnosis, provide objective data, and enhance protocol compliance. Ranked by clinical utility and evidence strength.
Recommended Products/Services:
- Dexcom Stelo (FDA-cleared OTC, 2024) - $99/month for non-diabetics
- Freestyle Libre 3 - prescription required, insurance may cover
- Levels Health CGM program - $199-399/month with coaching
- Nutrisense CGM + dietitian support - $225-350/month
Key Benefits:
- Identifies glucose nadirs <70 mg/dL correlating with brain fog onset
- Reveals 30-90 minute post-meal crash patterns
- Quantifies impact of specific foods on YOUR glucose response
- Tracks overnight glucose stability affecting morning cognition
Important Limitations: Dexcom Stelo NOT designed for hypoglycemia alerts (safety limitation). Prescription CGMs like Freestyle Libre provide low-glucose warnings
Evidence Base: CGM studies show reactive hypoglycemia occurs 30-40 min post-peak in high-carb meals, with glucose drops to 65 mg/dL average
→ Use for 2-4 weeks during elimination protocol to build glucose response database
Recommended Products/Services:
- Everlywell Food Sensitivity Test - $159 (96 foods, IgG)
- 5Strands Food Intolerance Test - $118-198 (760+ items tested)
- Viome Gut Intelligence Test - $129 (microbiome + food recommendations)
- Cyrex Array 3X - $325-425 (gluten/wheat reactivity, 24 markers) - Clinical gold standard
- ALCAT Food Sensitivity Panel - $295-995 (professional test, 200+ foods)
Key Benefits:
- Identifies hidden sensitivities beyond obvious symptoms
- Measures IgG delayed responses (24-72 hour reactions)
- Provides objective data to guide elimination priorities
- Zonulin testing available through some panels (gut permeability marker)
Important Limitations: IgG testing controversy - some experts question clinical significance. Best used alongside elimination diet, not as sole diagnostic. False positives/negatives possible
Evidence Base: Food sensitivities trigger IgE, IgG1, IgG2a antibodies, increasing TNF-α, IL-6 in brain tissue. 89% CD and 95% NCGS report neurocognitive symptoms
→ Consider if elimination diet is overwhelming or if you suspect multiple sensitivities. Cyrex Array 3X is gold standard for gluten reactivity
Recommended Products/Services:
- Cara Care - Free/Premium ($9.99/mo) - IBS and food sensitivity tracking
- MySymptoms Food Diary - $7.99 one-time - Comprehensive symptom correlations
- Ate Food Journal - Free - Photo-based tracking with mood/energy
- MyFitnessPal - Free/Premium - Macros + custom symptom tags
- See How You Eat - Free - Visual food journal with timestamps
Key Benefits:
- Tracks symptom onset time (critical for identifying 2-6 hour delayed reactions)
- Correlates specific foods with brain fog severity (1-10 scale)
- Identifies patterns across days/weeks (e.g., cumulative gluten exposure)
- Export data to share with healthcare providers
What to Look For: Look for: timestamp tracking, symptom severity scales, meal photo uploads, export functionality, custom tags for 'brain fog' 'energy' 'focus'
→ Essential during elimination and reintroduction phases. Document EVERY meal with symptom check-ins at 2hr, 6hr, 24hr post-meal
Template Contents:
- Daily meal log with time, foods, portion sizes
- Symptom severity tracker (brain fog, energy, mood, digestion) - 1-10 scale
- Glucose readings (if using CGM) - fasting, post-meal peaks, nadirs
- Sleep quality and duration log
- Stress level tracking (impacts glucose and symptoms)
- Bowel movement log (gut-brain axis connection)
- Reintroduction challenge protocol worksheet
- Week-by-week summary and pattern identification section
Key Benefits:
- Structured format ensures consistent data collection
- Physical act of writing enhances awareness and compliance
- No app required - accessible to all users
- Comprehensive view of all variables affecting brain fog
Format: Fillable PDF + Excel spreadsheet with auto-calculations for pattern detection
→ Download and print before starting elimination protocol. Complete after EVERY meal and at bedtime. Review weekly for patterns
Recommended Products/Services:
- PlateJoy - $12.99/mo - Custom meal plans for food sensitivities with grocery lists
- Mealime - Free/Premium ($5.99/mo) - Filter gluten, dairy, etc. with 15-min recipes
- Eat This Much - Free/Premium ($8.99/mo) - Automated meal planning with macro targets
- Paprika Recipe Manager - $4.99 one-time - Save recipes, filter by tags, meal planning
Key Benefits:
- Eliminates decision fatigue during restrictive elimination phase
- Ensures balanced macros (protein/fat/carb ratios) for glucose stability
- Generates grocery lists filtered for trigger foods
- Recipe database pre-filtered for common sensitivities
What to Look For: Must support multiple simultaneous exclusions (gluten AND dairy AND sugar). Look for low-GI recipe filters. Macro tracking essential
→ Invest in one app for Week 1 to reduce overwhelm. PlateJoy highest-rated for elimination diets specifically
Recommended Products/Services:
- Histamine Intolerance Blood Test - $99-189 (measures DAO levels + histamine)
- Available through: Diagnostic Solutions Lab, Doctor's Data, US Biotek
Key Benefits:
- Identifies if high-histamine foods are contributing to brain fog
- DAO <10 U/mL indicates histamine intolerance risk
- Guides targeted elimination of fermented foods, aged cheeses, alcohol
Evidence Base: Excess histamine crosses BBB, activates H3 autoinhibitory receptors causing neuronal 'shutdown' and fog. Associated with ASD, MCAS, POTS, fibromyalgia
→ Consider if you react to wine, aged cheese, fermented foods, or leftovers with immediate brain fog
Quick-Win Solutions (Start Today)
While the full elimination protocol provides comprehensive diagnosis, these evidence-based interventions can be implemented immediately to reduce postprandial brain fog. Each has been validated in clinical research and provides measurable benefit within days to weeks.
Action:
Always pair carbohydrates with protein (20-30g) and healthy fat (10-15g) to blunt glucose spike
Impact: Reduces peak glucose by 30-40% and prevents reactive hypoglycemia crash
Example:
Apple → Apple + 2 Tbsp almond butter. Toast → Skip toast, have eggs + avocado instead
Action:
Eat every 3-4 hours during waking hours. Never exceed 5 hours between meals
Impact: Prevents glucose nadirs that trigger brain fog and maintains neurotransmitter synthesis
Example:
Breakfast 7am → Snack 10:30am → Lunch 1pm → Snack 4pm → Dinner 7pm
Action:
Take 10-15 minute walk immediately after high-carb meals (or within 30 min)
Impact: Reduces postprandial glucose spike by 20-30% via muscle glucose uptake
Example:
After lunch, walk around block or do light household tasks before returning to desk
Action:
Consume 1 Tbsp apple cider vinegar in water 10-15 minutes before high-carb meals
Impact: Reduces postprandial glucose spike by ~20% via delayed gastric emptying
Example:
Before dinner: 1 Tbsp ACV + 8oz water + squeeze of lemon. Wait 10 min, then eat
Action:
Eat protein first in meal sequence, then vegetables, then carbohydrates last
Impact: Reduces glucose spike by 40-50% compared to carb-first eating. Enhances satiety
Example:
Dinner plate: Eat chicken first, then broccoli, then sweet potato last
Action:
Add 1-2 tsp Ceylon cinnamon to breakfast daily (smoothies, oatmeal, yogurt)
Impact: Improves insulin sensitivity, reduces fasting glucose by 10-29 mg/dL in some studies
Example:
Sprinkle on berries, mix into nut butter, add to coffee or tea
Action:
Drink 16-20oz water immediately upon waking, then 8oz every 2 hours until 6pm
Impact: Even 2% dehydration impairs cognitive function. Morning hydration supports cortisol-glucose regulation
Example:
6am: 16oz water + electrolytes → 8am: breakfast → 10am: 8oz water → repeat
Action:
Remove soda, juice, sweetened coffee, alcohol as immediate priority before food elimination
Impact: Liquid sugars cause fastest glucose spikes (GI 90-110). Alcohol has multi-mechanism brain impact
Example:
Replace morning juice with whole fruit. Replace afternoon soda with sparkling water + berries
When to See a Doctor About Postprandial Brain Fog
- Brain fog accompanied by severe headache, confusion, or fever (possible infection/inflammation)
- Symptoms persist despite 4+ weeks of strict elimination diet (suggests non-food cause)
- Progressive cognitive decline over weeks/months (evaluate for dementia, thyroid, B12 deficiency)
- Brain fog with unexplained weight loss >10 lbs (rule out celiac disease, IBD, diabetes)
- Severe reactive hypoglycemia with glucose <55 mg/dL (evaluate for insulinoma, Addison's disease)
- Brain fog after head injury or with neurological symptoms (weakness, vision changes, seizures)
- Symptoms with chronic diarrhea, bloody stools, or severe abdominal pain (evaluate for IBD, celiac)
- Concurrent depression, anxiety, or suicidal thoughts (psychiatric evaluation needed)
- Brain fog with heart palpitations, chest pain, or shortness of breath (rule out cardiac issues)
- Postural symptoms (worse when standing) with brain fog (evaluate for POTS, dysautonomia)
If postprandial brain fog persists despite 4 weeks of strict elimination diet, request comprehensive evaluation including:
- Metabolic panel: Fasting glucose, A1C, insulin, HOMA-IR (insulin resistance), oral glucose tolerance test with insulin levels
- Thyroid function: TSH, free T3, free T4, thyroid antibodies (hypothyroidism causes brain fog)
- Nutritional deficiencies: B12, folate, vitamin D, iron panel (ferritin, TIBC, serum iron)
- Celiac screening: Tissue transglutaminase IgA, total IgA, deamidated gliadin peptide antibodies
- Inflammatory markers: hsCRP, ESR, homocysteine
- Sleep evaluation: Consider sleep study if snoring, daytime fatigue, or witnessed apneas (sleep apnea causes brain fog)
Frequently Asked Questions
Timeline varies by mechanism: Reactive hypoglycemia improvements occur within 24-48 hours of blood sugar stabilization. Gluten-related fog may take 3-14 days to clear as zonulin levels normalize and intestinal inflammation reduces. Dairy-related casomorphin effects typically clear within 3-7 days. Histamine intolerance symptoms can improve within 1-3 days of strict elimination. Most people report noticeable clarity improvements by day 5-7 of the elimination protocol, with peak improvements at 2-4 weeks. If no improvement after 4 weeks of strict compliance, consider non-food causes (thyroid, sleep apnea, nutrient deficiencies, medications).
While sequential single-food elimination seems less overwhelming, it significantly extends diagnosis time (7 foods × 3-day testing = 21+ days just for reintroduction) and makes interpretation difficult if you're reacting to multiple foods simultaneously. The comprehensive elimination approach recommended here follows clinical protocols (NIH, Cleveland Clinic) because: (1) It creates a 'clean slate' baseline to accurately assess reintroductions, (2) Multiple sensitivities often coexist (e.g., gluten + dairy in 40% of cases), (3) Cumulative inflammation from multiple triggers may prevent symptom resolution if only one food is removed. However, if the full protocol is too restrictive, prioritize eliminating refined sugars and gluten first (highest impact foods) for 2 weeks, then reassess.
Symptoms alone can guide dietary changes, but CGM provides objective data that transforms guesswork into precision. Key advantages: (1) Identifies asymptomatic glucose drops—some people have blunted hypoglycemia awareness and don't feel crashes until glucose is very low, (2) Quantifies YOUR specific food responses—what spikes one person may not spike another (personalized nutrition), (3) Reveals timing patterns—pinpoints whether fog occurs at glucose nadir, during rise, or during fall, (4) Validates interventions—shows whether meal combinations actually stabilize your glucose. CGM studies document reactive hypoglycemia nadirs averaging 65 mg/dL at 30-90 min post-high-GI meals. For budget-conscious approach: try 1 month of CGM ($99-199) during elimination protocol to build your food response database, then continue without it using lessons learned.
Food sensitivity testing is controversial with important limitations: IgG antibodies may represent normal immune exposure rather than pathology (you may have IgG to foods you tolerate well). False positives are common. However, comprehensive panels can identify unexpected sensitivities and provide structure for elimination diets. Evidence-based approach: (1) IgG tests are screening tools, NOT diagnostic—must be validated with elimination/reintroduction, (2) Cyrex Array 3X for gluten reactivity has strongest clinical validation ($325-425), (3) DAO enzyme testing for histamine intolerance is more actionable than general IgG panels, (4) Best use case: if you're overwhelmed by elimination diet and need prioritization guidance. Most cost-effective strategy: Start with 2-week elimination protocol ($0) before investing in testing. If elimination diet is unclear or you suspect 10+ sensitivities, then consider testing.
Withdrawal symptoms during days 2-5 are common and expected, especially from sugar, gluten, dairy, and caffeine (if eliminated). Mechanisms: (1) Casomorphin withdrawal—dairy-derived opioid peptides cause actual withdrawal when removed, (2) Blood sugar adaptation—body adjusting from glucose roller coaster to stable levels, (3) Gut microbiome shift—bacteria that fed on eliminated foods die off, releasing endotoxins (Herxheimer reaction), (4) Caffeine withdrawal if coffee/tea was reduced. Typical symptoms: headache, irritability, fatigue, cravings, temporary brain fog worsening. Management: (1) Hydrate aggressively (2.5-3L daily) to clear metabolic byproducts, (2) Ensure adequate calories and protein—don't restrict calories during elimination, (3) Gentle movement like walking to support lymphatic clearance, (4) Electrolytes (sodium, potassium, magnesium), (5) Expect improvement by day 6-7. If severe symptoms or worsening after day 7, consult provider.
Yes—reactive hypoglycemia (RH) occurs in three forms, all in non-diabetic individuals: (1) Idiopathic RH (most common)—glucose drops at 180 min post-meal due to exaggerated insulin response, cause unknown, (2) Alimentary RH—occurs within 120 min after gastric surgery (dumping syndrome) but can occur in susceptible individuals, (3) Late RH—glucose drops at 240-300 min, associated with early insulin resistance or prediabetes. You can have normal fasting glucose, normal A1C, and still experience postprandial crashes. Risk factors: high-carb diet, insulin resistance (even subclinical), family history of diabetes, PCOS, history of gestational diabetes, chronic stress (cortisol dysregulation). CGM studies show RH glucose nadirs <70 mg/dL within 30-90 minutes after high-GI meals in otherwise healthy individuals. The brain, consuming 20% of body glucose, is exquisitely sensitive to these fluctuations even when they're 'subclinical' by standard testing.
Duration depends on mechanism and severity: (1) Reactive hypoglycemia—permanent dietary modification to low-GI, protein-balanced meals; high-GI foods will always trigger crashes, (2) Gluten sensitivity/celiac—permanent elimination if diagnosed; even small amounts trigger zonulin and inflammation, (3) Dairy sensitivity—trial reintroduction after 3-6 months of gut healing; some people regain tolerance, especially if sensitivity was secondary to leaky gut, (4) Histamine intolerance—may improve after 3-6 months if underlying cause (gut dysbiosis, DAO insufficiency) is addressed; may tolerate moderate histamine after healing, (5) Processed food additives—permanent minimization recommended; no health benefit to consuming excitotoxins. General principle: After 3-6 months of elimination and gut healing (L-glutamine, bone broth, probiotics, anti-inflammatory diet), can trial reintroduction of non-gluten triggers one at a time. If symptoms return, continue avoidance. Some sensitivities resolve (dairy, histamine), others are permanent (celiac, severe hypoglycemia response).
Key distinguishing features: (1) TIMING—Postprandial brain fog is temporally linked to meals (30 min-6 hours after eating specific foods), while CFS/ME is persistent and not meal-triggered, (2) POST-EXERTIONAL MALAISE—CFS/ME features severe symptom worsening after physical/mental exertion lasting 24+ hours (cardinal feature); food-triggered fog doesn't have this pattern, (3) RESPONSE TO ELIMINATION—Food-related fog improves significantly within 2-4 weeks of trigger food elimination; CFS/ME may improve somewhat but doesn't resolve with dietary changes alone, (4) ASSOCIATED SYMPTOMS—CFS/ME includes unrefreshing sleep, orthostatic intolerance, widespread pain, sore throat, tender lymph nodes; postprandial fog is primarily cognitive with possible digestive symptoms. However, food sensitivities can worsen CFS/ME, and many CFS/ME patients have comorbid food intolerances. If you have severe, persistent fatigue with post-exertional malaise regardless of diet, pursue CFS/ME evaluation while also addressing food triggers.
Related Topics
The Bottom Line
Postprandial brain fog is a measurable, reversible symptom caused by food-induced metabolic and inflammatory disruptions. The seven primary trigger foods—refined carbohydrates, gluten, dairy, processed additives, high-histamine foods, alcohol, and high-GI foods—operate through distinct mechanisms including reactive hypoglycemia, zonulin-mediated barrier disruption, inflammatory cytokine cascades, and neurotransmitter dysregulation.
- Reactive hypoglycemia (glucose crashes to <70 mg/dL within 30-90 min post-meal) is the most common cause, affecting brain glucose availability and causing immediate cognitive impairment
- Gluten sensitivity triggers zonulin release in 89-95% of sensitive individuals, disrupting intestinal and blood-brain barrier tight junctions, facilitating neuroinflammation
- The 2-week elimination protocol (Week 1: comprehensive elimination, Week 2: systematic reintroduction) is the gold standard diagnostic approach with clinical validation
- Glucose-stabilizing meal combinations (20-30g protein + healthy fats + low-GI carbs + fiber) prevent reactive hypoglycemia and maintain 3-5 hour cognitive energy
- CGM technology (Dexcom Stelo OTC, $99/month) provides objective glucose data to identify personal trigger foods and validate interventions, though not required for protocol success
- Quick-win interventions (never eat naked carbs, post-meal movement, vinegar pre-loading, protein front-loading) provide immediate benefit while comprehensive elimination proceeds
Most individuals experience noticeable cognitive improvement within 5-7 days of trigger food elimination, with peak clarity at 2-4 weeks. Reactive hypoglycemia improvements occur within 24-48 hours of blood sugar stabilization, while inflammatory mechanisms (gluten, dairy) require 3-14 days for symptom resolution. If brain fog persists despite 4 weeks of strict elimination compliance, comprehensive medical evaluation is warranted to rule out thyroid dysfunction, nutrient deficiencies, sleep disorders, or other underlying conditions.
Action Steps: (1) Download and print the food diary template, (2) Implement 2-3 quick-win strategies today (eliminate liquid sugar, never eat naked carbs, post-meal walks), (3) Begin full 2-week elimination protocol on a Monday to simplify meal planning, (4) Consider CGM for 1 month to build personalized glucose response database, (5) Seek medical evaluation if no improvement after 4 weeks or if red flag symptoms present.
